SOAP Note Example 1
At Speedy Template, You can download SOAP Note Example 1 . There are a few ways to find the forms or templates you need. You can choose forms in your state, use search feature to find the related forms. At the end of each page, there is "Download" button for the forms you are looking form if the forms don't display properly on the page, the Word or Excel or PDF files should give you a better reivew of the page.
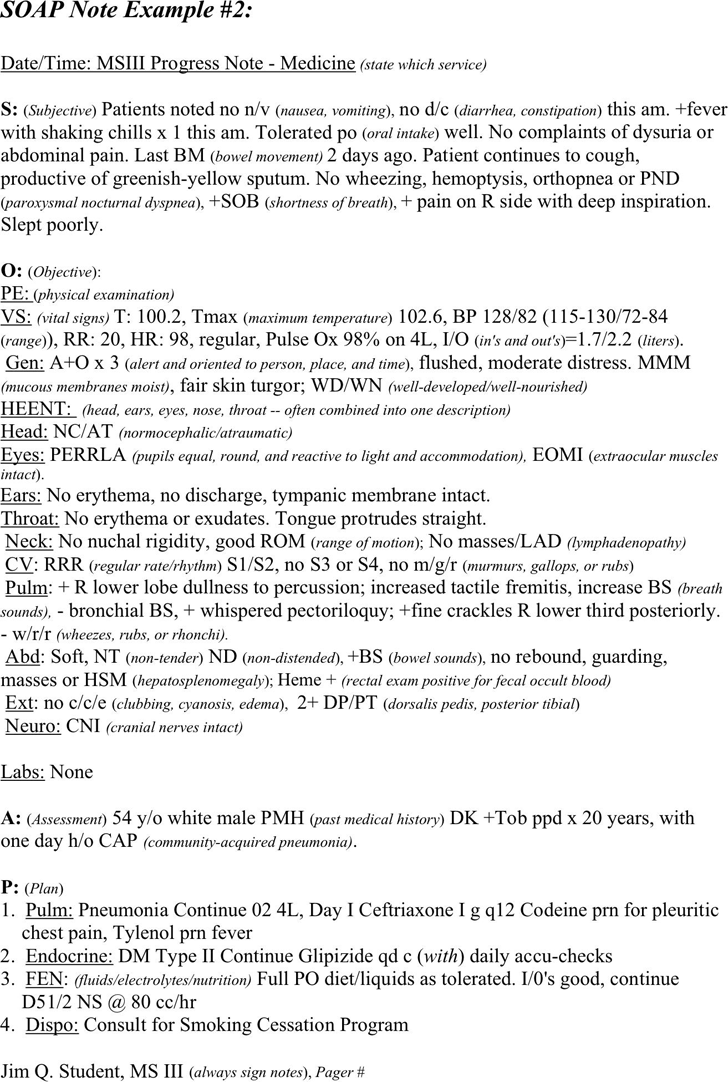
SOAP Note Example #2:
Date/Time: MSIII Progress Note - Medicine (state which service)
S:
(Subjective) Patients noted no n/v (nausea, vomiting), no d/c (diarrhea, constipation) this am. +fever
with shaking chills x 1 this am. Tolerated po
(oral intake) well. No complaints of dysuria or
abdominal pain. Last BM
(bowel movement) 2 days ago. Patient continues to cough,
productive of greenish-yellow sputum. No wheezing, hemoptysis, orthopnea or PND
(paroxysmal nocturnal dyspnea), +SOB (shortness of breath), + pain on R side with deep inspiration.
Slept poorly.
O:
(Objective):
PE: (physical examination)
VS: (vital signs) T: 100.2, Tmax (maximum temperature) 102.6, BP 128/82 (115-130/72-84
(range)), RR: 20, HR: 98, regular, Pulse Ox 98% on 4L, I/O (in's and out's)=1.7/2.2 (liters).
Gen:
A+O x 3 (alert and oriented to person, place, and time), flushed, moderate distress. MMM
(mucous membranes moist), fair skin turgor; WD/WN (well-developed/well-nourished)
HEENT:
(head, ears, eyes, nose, throat -- often combined into one description)
Head: NC/AT (normocephalic/atraumatic)
Eyes:
PERRLA (pupils equal, round, and reactive to light and accommodation), EOMI (extraocular muscles
intact).
Ears:
No erythema, no discharge, tympanic membrane intact.
Throat:
No erythema or exudates. Tongue protrudes straight.
Neck:
No nuchal rigidity, good ROM (range of motion); No masses/LAD (lymphadenopathy)
CV
: RRR (regular rate/rhythm) S1/S2, no S3 or S4, no m/g/r (murmurs, gallops, or rubs)
Pulm
: + R lower lobe dullness to percussion; increased tactile fremitis, increase BS (breath
sounds),
- bronchial BS, + whispered pectoriloquy; +fine crackles R lower third posteriorly.
- w/r/r
(wheezes, rubs, or rhonchi).
Abd
: Soft, NT (non-tender) ND (non-distended), +BS (bowel sounds), no rebound, guarding,
masses or HSM
(hepatosplenomegaly); Heme + (rectal exam positive for fecal occult blood)
Ext: no c/c/e (clubbing, cyanosis, edema), 2+ DP/PT (dorsalis pedis, posterior tibial)
Neuro:
CNI (cranial nerves intact)
Labs:
None
A:
(Assessment) 54 y/o white male PMH (past medical history) DK +Tob ppd x 20 years, with
one day h/o CAP
(community-acquired pneumonia).
P:
(Plan)
1. Pulm:
Pneumonia Continue 02 4L, Day I Ceftriaxone I g q12 Codeine prn for pleuritic
chest pain, Tylenol prn fever
2. Endocrine:
DM Type II Continue Glipizide qd c (with) daily accu-checks
3. FEN
: (fluids/electrolytes/nutrition) Full PO diet/liquids as tolerated. I/0's good, continue
D51/2 NS @ 80 cc/hr
4. Dispo:
Consult for Smoking Cessation Program
Jim Q. Student, MS III
(always sign notes), Pager #
SOAP Note Example 1


